by Michelle C. Arnett, MS, RDH, and Yvette Reibel, EdD, LDH
October 7, 2024
This case has been prepared for publication during National Dental Hygiene Month 2024. The content is revealed as clues in email and on social media, with the full clues, case and care presented here. The case follows the ADHA Standards for Clinical Dental Hygiene Practice and incorporates a clinically supported solution from Colgate.
Initial Clues and Assessment
A 21-year-old female patient presented for a routine prophylaxis. Examination and clinical assessments reveal mobility, sensitivity, and erythematous gingival tissue on maxillary central incisors.
Patient History

Extraoral images of 21-year-old patient
The patient was a college student who worked part time during the school year and required time off from work to attend dental appointments. She has been a patient of the clinic since age 14 and completed her orthodontic treatment in 2018. The patient has dental insurance coverage but has a co-pay for most treatments. The patient’s medical and dental history included asthma, which was controlled with an albuterol inhaler, use of electronic cigarettes, bruxism and grinding. The frequency of electronic cigarette use was documented in the patient electronic health record (EHR) stating the patient used a 6.5 mL packet (2,000 puffs) containing 50 mg of nicotine salt every three days. Patient’s chief complaint is that she has pain and sensitivity around teeth #8 and #9. Patient was also concerned about a relapse of a diastema after she had lost her orthodontic retainers.

Intraoral Image, Lingual #8-9
In a 2020 dental hygiene visit, clinical findings were Class I mobility #8 and an erythematous fibroma on the buccal and lingual between #8 and #9. A periapical radiograph revealed possible fracture between #8 and #9. Endodontic testing for #9 was positive to percussion, palpation, and mobility. An orthodontic consultation occurred and the treatment plan included fabrication and delivery of an Essix retainer to stabilize tooth #9. The patient was also consulted to stop using the DIY rubber band method to close the diastema between #8 and #9.
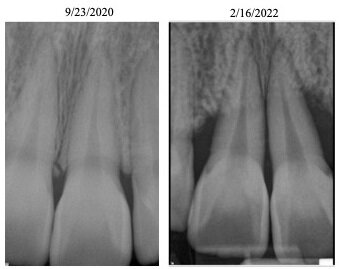
Periapical radiograph of tooth #9 obtained Sept. 2020 compared to Feb. 2022
In a 2022 routine dental hygiene visit, clinical periodontal findings worsened, and the patient was classified with periodontitis localized Stage IV Grade C with heavy subgingival calculus. Specific to #8 and #9, Class 3 mobility was present on #8 and exudate during probing on the mesial-facial of #9. A periodontal consultation occurred and the treatment plan included smoking cessation, localized scaling and root planing (SRP) #8, #9, #14, and #15, splitting teeth #8 and #9, occlusal adjustment to remove excursive inference, oral hygiene instruction (brushing and flossing twice daily), minimize biting with anterior teeth, and to cease using a DIY rubber band method to close the diastema.
Current Patient Homecare Routine
Patient reported brushing once a day and occasionally flossing. No other adjuncts were reported by the patient. The patient reported using rubber bands as a ‘do-it-yourself’ (DIY) method to close the diastema that has appeared since she lost her orthodontic retainer. The DIY rubber method was something she saw on social media and started doing for her relapsed diastema since she lost her orthodontic retainer in 2018.
Diagnosis
Clues to inspire diagnosis and knowledge application to formulate the differential diagnosis for the advanced bone loss of 65-80% around #8 and #9 included 1) bone loss as a result of occlusal disease (bruxism), 2) bone loss resulting from orthodontic forces, and 3) bone loss due to home applied rubber bands as a DIY orthodontic method.
Clues
- What factors contribute to bone loss of the periodontium?
- What factors contribute to worsening oral health?
- What is the role of plaque biofilm on the progression of periodontal disease?
- How does bruxism impact periodontal hard and soft structures?
- Why is it concerning for Stage IV Grade C periodontitis in a 21-year-old patient?
Dental Hygiene Diagnosis
21-year-old female with a history of vaping, poor plaque biofilm control, bruxism, and Stage IV Grade C periodontitis.
Planning
Several specialty consultations were completed to assess the current clinical condition and the rapid advancement of bone loss and periodontal condition. Several factors were discussed including the patient’s willingness to cease using rubber bands at home, rapid advancement of bone loss and mobility, increasing periodontal pockets with exudate present, restorability of function, and overall prognosis of the maxillary central incisors.
Orthodontic forces induce periodontal bone loss and root resorption.1,2 An experimental study published in the Journal of Periodontology states that orthodontic movement increases the progression of periodontal breakdown by upregulating proinflammatory cytokines, specifically Interleukin-1B and Tumor Necrosis Factor- a.3 Another study done by the International Journal of Orthodontics and Dentofacial Orthopedics states that 90% of patients younger than 30 show dehiscence (reduced bone level) after orthodontic therapy.4
Since this patient has already gone through orthodontic treatment, her bone level was most likely reduced from normal.2 The addition of DIY rubber bands for tooth movement of #8 and #9 caused rapid bone loss of the periodontium.1-4 The patient also added trauma to the area by the use of rubber bands, this caused pain of the incisive papilla and the patient could not perform adequate home care resulting in inflammation and gingivitis which lead to periodontitis in the affected area.5
Prognosis: Poor to restore function due to advanced bone loss and mobility.
Implementation
Several specialty consultations were completed to assess the current clinical condition and the rapid advancement of bone loss and periodontal condition. Several factors were discussed.
The treatment plan selection was to extract teeth #8 and #9, bone graft, and place two implants, abutments, and crowns to restore function and aesthetics. During the extraction of tooth #9, it was determined that there was a residual rubber band affixed to the apical one-third of tooth #9. Upon further examination, there was significant glandular tissue surrounding the rubber band. Post-surgical instructions included the use of acetaminophen and ibuprofen regimen for pain management, chlorhexidine rinse and amoxicillin for microbial control. Currently the bone graft and implant placement has been completed and the patient is in the healing phase.
The patient’s response to treatment was satisfaction that function and aesthetics would be restored. She accepted the homecare recommendations of brushing twice a day, and flossing daily once healing has occurred. The patient also reported that she stopped using electronic cigarettes for 6 months prior to the bone grafting procedure. Next phase will be impressions and fabrication of the implant crowns and seat the crowns to the implant abutment.
Home care recommendations could include a powered toothbrush, like Colgate® Hum with the app tracking, to decrease the amount of plaque biofilm present thus resulting in reduced bleeding present. Another recommendation is to use floss daily and the patient could benefit from using Colgate® Total Plaque Pro-Release, and Colgate® PerioGard in plaque control.
____________________________________

Help prevent caries and white spots before they start with Colgate® PreviDent 5000 ppm Ortho Defense (1.1% Sodium Fluoride) toothpaste and Colgate® Phos•Flur® Ortho Defense® Rinse – Sodium Fluoride and Acidulated Phosphate.
To order contact your Colgate Territory Manager or call 1-800-2COLGATE (1-800-226-5428) Monday – Thursday (7:30 am – 5:30 pm CST) Friday (7:30 am – 4:30 pm CST) to speak to a customer service specialist.
Important Safety Information
PreviDent® 5000 ppm Ortho Defense Toothpaste: Do not swallow. Keep out of reach of children. Acute burning in the mouth and sore tongue may be experienced by some individuals. If accidental ingestion occurs, side effects may include nausea, vomiting, diarrhea, and abdominal pain. See Package Insert for additional safety information.
STATUTORY PRICE DISCLOSURE FOR COLORADO PRESCRIBERS: In accordance with the Colorado Wholesale Acquisition Cost Disclosure Law (Colorado Revised Statutes Section 12-42.5-308), Colgate Oral Pharmaceuticals, Inc. is disclosing to you, as an authorized prescriber of prescription drugs in Colorado, certain required pricing information for Colgate Oral Pharmaceuticals, Inc. marketed prescription drugs. Please visit this webpage to access this price disclosure information.
STATUTORY PRICE DISCLOSURE FOR CONNECTICUT PRESCRIBERS: In accordance with the Connecticut Public Act No. 23-171, Colgate Oral Pharmaceuticals, Inc. is disclosing to you, as an authorized prescriber of prescription drugs in Connecticut, certain required pricing information for Colgate Oral Pharmaceuticals, Inc. marketed prescription drugs. Please visit this webpage to access this price disclosure information.
____________________________________
Evaluation
Evaluation occurred at multiple time points due to failed treatment. The localized SRP #8, #9, #14, and #15 did not reduce probing depths (PD), bleeding on probing (BOP) or mobility. The splitting of teeth #8 and #9 was not completed to reduce mobility due to the rapid progression of bone loss. In fact, periodontal conditions worsened to support the treatment plan of extraction of #8 and #9 and restore function and aesthetics with implants.
Future evaluations to determine peri-implant health will be measured by annual radiographic bone levels, periodontal examination of PD, BOP and mobility classification of implants #8 and #9. Evaluation of oral hygiene behaviors (brushing and flossing) will be measured by patient’s self-report of frequency of compliance, plaque index and BOP. Evaluation of lifestyle behaviors will be measured by the patient’s self-report usage of electronic cigarettes.
Documentation
Documentation included patient consent for SRP, tobacco cessation, and OHI. After failed treatment, the patient consented for extraction of teeth #8 and #9 with bone grafting. Consent will need to be obtained for implant crown delivery. Future documentation needs to include periodontal clinical indicators of disease measured by annual radiographs, periodontal examination, plaque index, patient oral hygiene and periodontal maintenance compliance, and lifestyle behaviors (tobacco use). Documentation of the clinician’s future care includes 3-month periodontal maintenance, remaining tobacco free, twice daily brushing and flossing.
____________________________________
Article References
1 Kirschneck C, Fanghänel J, Wahlmann U, et al. Interactive effects of periodontitis and orthodontic tooth movement on dental root resorption, tooth movement velocity and alveolar bone loss in a rat model. Ann Anat. 2017 Mar:210:32-43.
2 Guo R, Zhang L, Hu M, et al. Alveolar bone changes in maxillary and mandibular anterior teeth during orthodontic treatment: A systematic review and meta‐analysis. Orthod Craniofac Res. 2021 May;24(2):165-79.
3 Boas Nogueira AV, Chaves de Souza JA, Kim YJ, et al. Orthodontic force increases interleukin-1β and tumor necrosis factor-α expression and alveolar bone loss in periodontitis. J Periodontol. 2013 Sep;84(9):1319-26.
4 Jäger F, Mah JK, Bumann A. Peridental bone changes after orthodontic tooth movement with fixed appliances: A cone-beam computed tomographic study. Angle Orthod. 2017 Sep;87(5):672-80.
5 Pellegrini G, Francetti L, Barbaro B, et al. Novel surfaces and osseointegration in implant dentistry. J Investig Clin Dent. 2018 Nov;9(4):e12349.
____________________________________
 Michelle C. Arnett, MS, RDH, currently serves as an Associate Professor in the Department of Primary Dental Care, Division of Dental Hygiene at the University of Minnesota (UMN) School of Dentistry (SOD). She has 20 years of clinical practice experience and nine years of experience in academics and research at the University of Michigan SOD and the UMN SOD. Her areas of research focus are motivational interviewing and periodontology. In addition to topics to enhance her teaching, student mentorship, and dental hygiene educator burnout. Michelle has taught Communications, Periodontology, and the Process of Care in Allied Oral Health: Clinical Application III and currently teaches Process of Care in Allied Oral Health: Clinical Application IV in the UMN SOD dental hygiene undergraduate program and Thesis I, II and the Capstone Track (I-IV) in the UMN dental hygiene graduate program. Her professional memberships include Sigma Phi Alpha-Nu Chapter, American Dental Hygienists’ Association (ADHA), and the American Dental Education Association (ADEA).
Michelle C. Arnett, MS, RDH, currently serves as an Associate Professor in the Department of Primary Dental Care, Division of Dental Hygiene at the University of Minnesota (UMN) School of Dentistry (SOD). She has 20 years of clinical practice experience and nine years of experience in academics and research at the University of Michigan SOD and the UMN SOD. Her areas of research focus are motivational interviewing and periodontology. In addition to topics to enhance her teaching, student mentorship, and dental hygiene educator burnout. Michelle has taught Communications, Periodontology, and the Process of Care in Allied Oral Health: Clinical Application III and currently teaches Process of Care in Allied Oral Health: Clinical Application IV in the UMN SOD dental hygiene undergraduate program and Thesis I, II and the Capstone Track (I-IV) in the UMN dental hygiene graduate program. Her professional memberships include Sigma Phi Alpha-Nu Chapter, American Dental Hygienists’ Association (ADHA), and the American Dental Education Association (ADEA).
 Yvette Reibel, EdD, LDH, currently serves as an Assistant Professor in the Department of Primary Dental Care, Division of Dental Hygiene at the University of Minnesota (UMN) School of Dentistry (SOD). She has 20 years of clinical practice experience and nine years of experience in academics and research at the UMN SOD. Her areas of research focus are obstructive sleep apnea, curriculum development and assessment. Yvette has taught Dental Hygiene Preclinic and the Process of Care in Allied Oral Health: Clinical Application II and currently teaches Pharmacology, Research Methods, and Process of Care in Allied Oral Health: Clinical Application VI Capstone in the UMN SOD dental hygiene undergraduate program and Curriculum Development and Design, Didactic Student Teaching, Clinicals Administration, and Thesis III: Data Analysis in the UMN dental hygiene graduate program in addition to being the program director.
Yvette Reibel, EdD, LDH, currently serves as an Assistant Professor in the Department of Primary Dental Care, Division of Dental Hygiene at the University of Minnesota (UMN) School of Dentistry (SOD). She has 20 years of clinical practice experience and nine years of experience in academics and research at the UMN SOD. Her areas of research focus are obstructive sleep apnea, curriculum development and assessment. Yvette has taught Dental Hygiene Preclinic and the Process of Care in Allied Oral Health: Clinical Application II and currently teaches Pharmacology, Research Methods, and Process of Care in Allied Oral Health: Clinical Application VI Capstone in the UMN SOD dental hygiene undergraduate program and Curriculum Development and Design, Didactic Student Teaching, Clinicals Administration, and Thesis III: Data Analysis in the UMN dental hygiene graduate program in addition to being the program director.



