by Jo-Anne Jones, RDH, FIADFE
April 11, 2025
If you have ever had a diagnosis from a medical doctor that leaves your life temporarily hanging in the balance, you will truly appreciate the emotional impact the news of oral or oropharyngeal cancer has on an individual.
April is Oral Cancer Awareness Month where our attention turns towards this insidious disease, but all too often, that focus fades, while the threat continues to escalate. Here are the sobering facts: the rates of oral and oropharyngeal cancers continue to rise with a 35% increase over the last decade alone. (See Table 1)
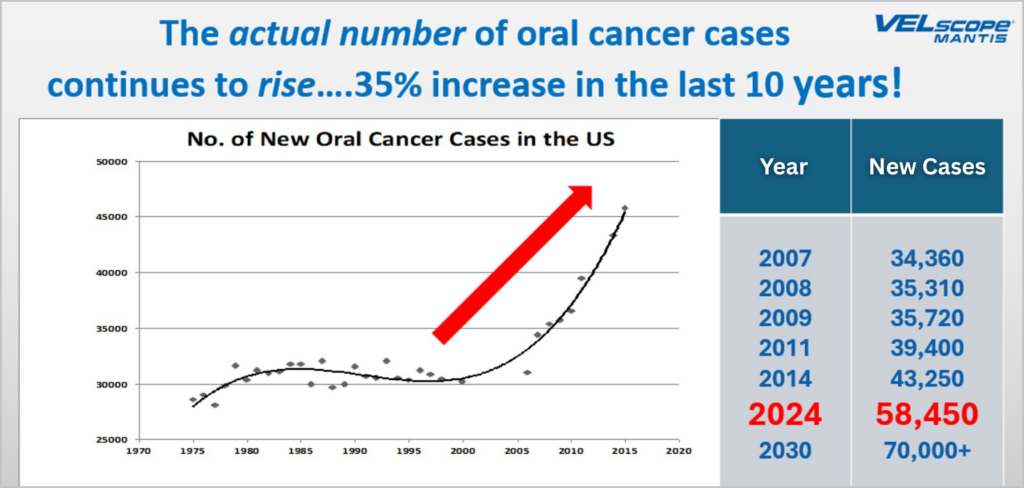
Table 1: Rise in oral cancer cases. Image used with permission.
Almost 60,000 Americans will be diagnosed with oral or pharyngeal cancer in 2025 which translates to 1 person diagnosed every 10 minutes1 claiming the lives of over 12,000 Americans. Of those 60,000 newly diagnosed individuals, only slightly more than half will be alive in 5 years. The “lucky” ones who survive have endured doses of radiation far exceeding what the human body is meant to withstand coupled often with chemotherapy, possibly immunotherapy, and the placement of a feeding tube early on in treatment to sustain nutritional requirements. Suicide rates are twice as high as for other cancers.2,3 There are many reasons for this including a ‘new normal’ which may include facial disfigurement, debilitating salivary depletion causing difficulty both in swallowing and speaking, social isolation, continuous onslaught of painful oral lesions, and fear of recurrence, to name a few.
The average age at diagnosis for both oral cavity cancer and oropharyngeal cancer is 64, however, we are now seeing a greater number of cases in males younger than 55 years of age. The stories possess an eerie commonality. Today’s oral and oropharyngeal cancer victim is surprisingly unpredictable with approximately 20% being non-smokers, non-drinkers, living a healthy lifestyle. As the number of oral and oropharyngeal cancer rates continue to rise, we can no longer rely on outdated knowledge and antiquated screening methods.
Here are the top 5 things we need to know to re-ignite our commitment to earlier discovery.
1. Know the Trends Driving the Increase
Most people are unaware of the driving force behind the escalating trajectory of oropharyngeal cancer cases. The COVID pandemic did not help matters either with interruptions in both dental and medical care.4,5 Diagnoses were delayed as well as subsequent treatment all contributing to a dramatic increase in risk for both oral cavity and oropharyngeal cancer. While use of vaping products has been advocated as harm reduction alternatives to tobacco products, studies continue to reveal detrimental effects of carcinogenic additives.6 However, the foregoing is not the strongest contributor to the escalation of oropharyngeal cancers.
While the historical etiologic pathways of smoking and alcohol use are still prevalent particularly in oral cavity cancer, the culprit and secret killer related to oropharyngeal cancer, is the Human Papillomavirus (HPV). The 2nd biggest misconception is that HPV-related cervical cancer is the most common site for HPV-related cancer, when in fact the oropharynx is the prominent site and has been for over a decade.7 The CDC (Centers for Disease Control) state that HPV is the cause behind 60% to 70% of oropharyngeal cancers in the United States8 As the CDC also affirms, HPV is so common, that almost every sexually active adult will have one or more infections in a lifetime and most will be unaware. Most of those infected will clear the virus, however, for those afflicted with a persistent, high-risk HPV strain, the transformation to cancer is a very real threat.
2. Our Role in Education and Prevention
It is a very dangerous assumption to assume the patient in your chair to be low risk. The unintentional exclusion of cancer evaluation in younger patients or those who do not possess typical and historical risk factors is leading to delays in diagnosis and costing lives. In 2019, the ADA announced an expansion to its policy on oral cancer detection, recommending that dentists [and dental hygienists] perform routine examinations for oral cancer, including oropharyngeal cancer, for all patients.9,10 This change was brought about to align with concerns from the Centers for Disease Control and Prevention (CDC) over the escalating numbers of diagnosed cases of oropharyngeal cancer linked to the human papillomavirus (HPV) and low uptake of HPV vaccination for males.
Did you know that over 92% of all future HPV-attributable cancers can be prevented?11 The 9-valent Gardasil vaccine addresses all 9 of the HPV strains that could be cancer-causing. As dental professionals, we are powerfully situated to relay this information to the public. Become knowledgeable about the benefits of vaccination and those groups in our community who may be at risk regardless of age.
3. Effective Screenings and Subtle Life-Saving Symptoms
HPV-related oropharyngeal cancer has an affinity for lymphoid tissues presenting a further layer of complexity with clinical assessment. The HPV-related anatomical sites most commonly impacted are the tonsils, tonsillar crypts, soft palate, uvula, and the base of the tongue. The non-HPV positive tumors occur more frequently on the anterior portion of the tongue, floor of the mouth, hard palate, and buccal mucosa. The signs and symptoms that may be associated with oral and oropharyngeal cancer range from the obvious to the very subtle. Take the time to acquaint yourself with these life-saving symptoms.12
Over 2/3 of oral cancers are discovered in later stages greatly impacting survival rates and treatment outcomes.13 The principal of direct fluorescence visualization previously employed in the cervix, lungs and the colon, has the ability to identify abnormal mucosal changes at the basement membrane in earlier stages of development that may be otherwise be invisible with white light examination. With science supported technologies like VELscope Vx and OralID at our fingertips, we have the tools to detect oral cancer earlier. It begs the question as to why wouldn’t we use every advantage to give our patients the best chance at early discovery and better outcomes?
4. When to Refer
Persistence is KEY and never something to be ignored. Any lesion and/or symptom that persists beyond 14 days always warrants a secondary evaluation, whether that is interpreted to mean re-appointing to confirm resolution or referral for further microscopic evaluation. A ‘wait and watch’ attitude has claimed countless lives across North America and must stop.
5. Our Role in Patient Care Throughout the Journey
You may be one of the most important resources and comfort to the head and neck cancer patient. Managing oral side effects from treatment for many is worse than the cancer itself.
One of the greatest debilitating side effects of radiation treatment is dry mouth. Without adequate salivary flow, oral health is at tremendous risk. Furthermore, if xerostomia is not effectively managed, it can go far beyond significantly damaging a patient’s oral health and have a major impact on general health. There is one product on the market that has a strong differentiator and that is Aquoral®. Aquoral is a lipid-based solution reflecting the outcome of the Cochrane Database Systematic Review of all topical therapies.14 The lipid-based formulation is made up of oxidized glycerol triesters which differentiates from all other water-based over-the-counter oral sprays, rinses, and gels. The lipid-based formulation has the ability to bind to the oral cavity and throat by formation of a lipid film which limits loss of water, restores the viscoelasticity, and protects the oral mucosa.15
In conclusion, oral and oropharyngeal cancer screening is NOT a choice. It is our ethical responsibility. Our dental patients need to understand that this examination is not considered to be elective, but mandatory. We need to educate our patients to be keenly tuned into the health of their mouth by doing a self-examination between professional visits.16 As a colleague, I would challenge you to examine your present means of assessment for your patients and critically evaluate the level of care you are presently providing. If you have any part in early detection of this insidious disease, it will be a job well done and a gratification compared to none.
A 4-minute examination is all that is required of your time which may translate to a lifetime to one of your patients.
____________________________________
Resources
Cancer Prevention Through HPV Vaccination: An Action Guide for Dental Health Care Providers https://hpvroundtable.org/wp-content/uploads/2018/04/DENTAL-Action-Guide-WEB.pdf
Dr. Mike Milligan https://aquoralspray.com/head-amp-neck-cancer-insights-from-dr-mike-milligan-a-survivor/
Watch the Oral Cancer Screening Examination https://www.youtube.com/watch?v=q9kPdQMyU40&t=2s
Talking to Parents About HPV Vaccine https://www.cdc.gov/hpv/media/pdfs/2024/07/talking_to_parents_hpv.pdf
VELscope Training Centre https://velscope.com/training/
References
1American Cancer Society. “Key Statistics for Oral Cavity and Oropharyngeal Cancers.” American Cancer Society, 2025. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2025/2025-cancer-facts-and-figures-acs.pdf.
2Osazuwa-Peters, Nosayaba, Mark C. Simpson, Liang Zhao, Eric Adjei Boakye, Stephanie I. Olomukoro, Teresa Deshields, Travis M. Loux, Maria Pisu, and Mario Schootman. “Suicide Risk Among Cancer Survivors: Head and Neck Versus Other Cancers.” Cancer 124, no. 20 (2018): 4072-4079. https://www.ncbi.nlm.nih.gov/pubmed/30335190.
3“Oral Cancer Patients Are Thinking About Killing Themselves.” DrBicuspid.com. Accessed April 7, 2025. https://www.drbicuspid.com/dental-hygiene/oral-systemic-link/oral-cancer/article/15736016/oral-cancer-patients-are-thinking-about-killing-themselves.
4Nath, Sanchita, Jose Ferreira, Andrew McVicar, et al. “Rise in Oral Cancer Risk Factors Associated with the COVID-19 Pandemic Mandates a More Diligent Approach to Oral Cancer Screening and Treatment.” Journal of the American Dental Association (March 2022).
5North American Quitline Consortium. “Report on the Impact of the COVID-19 Pandemic on Smoking Cessation.” North American Quitline Consortium. https://cdn.ymaws.com/www.naquitline.org/resource/resmgr/reports-naqc/report_impact__of_covid-19_p.pdf.
6Herzog, Christian, Angela Jones, Isis Evans, Jessie R. Raut, Michal Zikan, David Cibula, Amanda Wong, Hermann Brenner, Rebecca C. Richmond, and Martin Widschwendter. “Cigarette Smoking and E-cigarette Use Induce Shared DNA Methylation Changes Linked to Carcinogenesis.” Cancer Research (March 19, 2024).
7Centers for Disease Control and Prevention. “Human Papillomavirus (HPV).” Centers for Disease Control and Prevention. Accessed April 7, 2025. https://www.cdc.gov/hpv/index.html.
8“HPV and Oropharyngeal Cancer.” Centers for Disease Control and Prevention. Accessed April 7, 2025. https://www.cdc.gov/cancer/hpv/oropharyngeal-cancer.html.
9“ADA Expands Policy on Oral Cancer Detection to Include Oropharyngeal Cancer.” Oral Health Group. Accessed April 7, 2025. https://www.oralhealthgroup.com/news/ada-expands-policy-on-oral-cancer-detection-to-include-oropharyngeal-cancer-1003945246/.
10“Cancer, Head and Neck.” American Dental Association. Accessed April 7, 2025. https://www.ada.org/resources/ada-library/oral-health-topics/cancer-head-and-neck.
11“HPV Vaccine Recommended to Prevent Cancer.” Centers for Disease Control and Prevention. August 22, 2019. https://archive.cdc.gov/www_cdc_gov/media/releases/2019/p0822-cancer-prevented-vaccine.html.
12“Know the Life-Saving and Subtle Symptoms of HPV-Related Oropharyngeal Cancer.” Oral Cancer Foundation. Accessed April 7, 2025. https://oralcancerfoundation.org/understanding/hpv/hpv-oral-cancer-facts/.
13Saka-Herrán, Catalina, Enric Jané-Salas, Antoni Mari-Roig, Adelaida Estrugo-Devesa, and José López-López. “Time-to-Treatment in Oral Cancer: Causes and Implications for Survival.” Cancers 13, no. 6 (March 16, 2021): 1321. https://doi.org/10.3390/cancers13061321.
14Furness, Susan, Helen V. Worthington, Gemma Bryan, Sarah Birchenough, and Richard McMillan. “Interventions for the Management of Dry Mouth: Topical Therapies.” Cochrane Library. Accessed April 7, 2025. https://www.cochrane.org/CD008934/ORAL_interventions-for-the-management-of-dry-mouth-topical-therapies.
15“Aquoral Spray.” Accessed April 7, 2025. https://aquoralspray.com/.
16″Check Your Mouth.” The Oral Cancer Foundation. Accessed April 7, 2025. https://checkyourmouth.org/wp/.
____________________________________
Jo-Anne Jones, RDH, FIADFE, is a respected thought leader and international, award-winning speaker, who has given over 1,000 presentations worldwide. Jo-Anne is a past honoree of DPR’s Top 25 Women in Dentistry and joins the 2025 Dentistry Today CE Leaders for the 15th consecutive year. A Fellowship Award with the International Academy for Dental Facial Esthetics was presented to Jo-Anne for her contributions to the field of dentistry. Her work focuses on urgent issues within the dental field, such as oral and oropharyngeal cancer screening and HPV awareness, highlighting the latest research and practical applications for dental professionals. A frank and open lecture style and a focus on direct knowledge translation have earned Jo-Anne many loyal followers both nationally and internationally.


